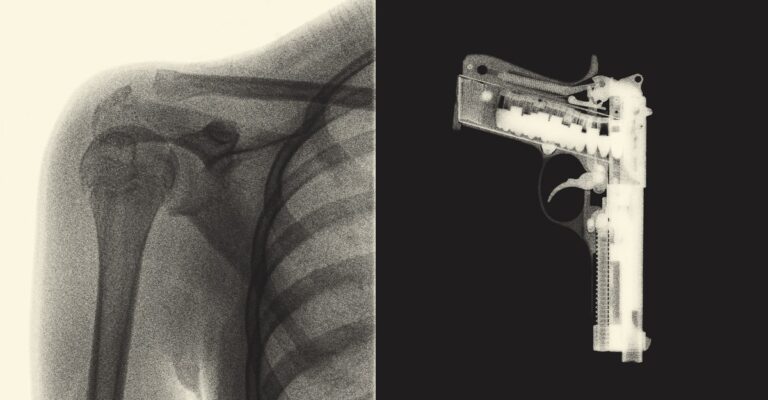
A man arrives at Northwell Health Hospital in Staten Island with a sprained ankle. Do you have any allergies? the doctor asks. How many alcoholic drinks do you drink each week? Can you use a firearm inside or outside your home? If the patient answers “yes” to the last question, someone on the patient’s care team explains that locking up firearms will make their home safer. She offered him a gun lock and a pamphlet with information about safe storage and the firearm’s safety class. And all this happened during a visit about his ankle.
Northwell Health is part of a growing movement of health care providers who want to treat firearm injuries as a public health issue and have the same conversations with patients about guns as they do about diet, exercise and sex. In recent years, White House declared gunshot injuries an epidemic, and the CDC and National Institutes of Health began funding prevention research.Meanwhile, dozens of medical society We agree that firearm injuries are a public health crisis and that health care providers must help stop it.
This could include asking patients about access to firearms and advising them to store them responsibly. “This is the same thing as encouraging people to wear their seat belts for exercise and not drink and drive,” said Emmy Betts, an emergency medicine physician and director of the University of Colorado Firearm Injury Prevention Initiative. told me. Unsecured guns may be accessible to children, people with dementia, or people with violent intentions. May increase Possibility of suicide? accidental injury Inside the house. Storing your gun safely National Rifle Association Safety Regulationsbut now 2016only about half of firearm owners reported doing so for all guns.
Several evidence It has been shown that when healthcare professionals counsel patients and provide them with locking devices, they develop safer storage habits. Doctors are now trying to figure out the best way to start the conversation. The doctor talks about sex, drugs, and even rock and roll (if your earphones are too loud). But for many firearm owners, guns are different.
Not long ago, leading doctors argued that if guns were causing so much harm, we should stop using them. In the 1990s, the director of the CDC’s Injury Center said that a public health approach to gun injuries meant rebranding guns as a dangerous vice, just like tobacco. “In the past, smoking was seen as a symbol of glamor, cool, sexy, macho,” he said. new york times “Now it’s dirty, dangerous, and forbidden,” the American Academy of Pediatrics said in the 2010s. advice They were to “never” have guns in the house because their presence greatly increases the risk of suicide or injury to children. (“Don’t buy guns,” the group bluntly warned.) And when asked, 2016 When it comes to who they turn to for advice on safe storage, gun owners ranked doctors second from the bottom and higher than celebrities.
Over the past few decades, some states have enacted laws that limit doctors’ ability to talk to patients about firearms and the information they can collect to allay privacy concerns among gun owners. In 2011, only Florida passed the most restrictive version, what doctors call a “gag law.” Six years later, a federal court invalidated it. But “I think gag orders, even if they’re not in effect right now, really scare people,” says Amy, an emergency psychiatrist and firearms injury prevention researcher at the University of California, Davis. Bernhorst told me.Just a little the study doctors, especially pediatrician—It is generally considered important to talk to patients about firearm safety, but in most cases, patients do not do it. As of 2019, 8 percent of firearm owners Their doctor said he had brought it up.
That year, Bernhorst, with state funding, launched the Bullet Point Project in California, a free curriculum that teaches health care professionals when and how to talk to patients about firearms. The program keeps politics and personal opinions out of the conversation and focuses on special reasons that require special attention, such as those with children, those experiencing domestic violence, or those living with someone with a cognitive disability. We instruct patients to ask questions only to patients who have It also suggests more realistic advice than “don’t buy guns.” Since the patient probably owns the gun for self-defense (the most common reason for owning a gun), they would think twice about unloading the gun, locking it up, and storing ammunition separately. Your healthcare provider may recommend a readily accessible lockbox instead.
Researchers are now testing whether the best outcomes are achieved when doctors only broach conversations about firearms when there is a clear reason to do so, or when doctors initiate conversations about firearms with doctors. ing. every Patient. Johns Hopkins University is trying a targeted approach, including talking about firearms and offering gun locks in case of trauma to pediatric patients. Meanwhile, Northwell Health, New York state’s largest health system, is asking everyone who visits some emergency departments about firearm use and offering locks to those who need them. Both of these efforts are federally funded studies that examine whether doctors feel confident enough to actually talk to their patients about this and whether those conversations will help people store their firearms more safely. This is a test to see if it leads to this.
Sandeep Kapur, an assistant professor of emergency medicine at Northwell Health who is helping implement the program, said universal screening means for doctors “no leeway in deciding who to ask and when.” Told. . So far, Northwell’s trial has tested about 45,000 patients, showing the approach can be scaled up. With this strategy, Kapur said, conversations about gun safety could eventually become as routine for patients as taking their blood pressure. Katherine Hoopes, a core faculty member at the Johns Hopkins Center for Resolving Gun Violence, said that when she was in her elementary pediatrics department, she included firearm safety in every health exam, just like bike helmets and seatbelts. I was incorporating it. (The American Academy of Pediatrics is still maintain The organization says the safest home for a child is one without guns, but now… It is recommended Pediatricians discuss safe storage with each family; curriculum Universal screening can also find people who might be missed by targeted approaches. Through screening questions, a team at Northwell University recently learned that a 13-year-old boy who came in with appendicitis had been threatened with a gun by bullies. He called in his parents, a team of social workers and the school to help.
But a patient in the ER with a sprained ankle may wonder why a doctor would ask about a firearm. “There’s no context,” Chris Barsotti, an emergency medicine physician and co-founder of the National Firearm Injury Reduction Medicine Foundation, told me. He said the firearms community remembers when “the CDC tried to destigmatize gun ownership,” so any move by health care workers to raise these issues requires nuance. In his opinion, these should be customized conversations. Betts, of the University of Colorado, believes that only raising the issue when patients are at risk, firearm safety may be in the background in other cases, such as in waiting rooms. . secure storage Pamphlet It is displayed alongside pamphlets on safe sex and posters on diabetes prevention.
According to one report, about half of patients who own firearms agree that there are times when it is appropriate for doctors to talk to patients about firearms. 2016 survey By Betts and colleagues.they are equal more It’s okay if you have children at home. The doctors I asked said that most of the time, these conversations go smoothly. But Betts’ research also found that 45% of patients who own firearms think doctors should never take them out. Paul Shea, a radiologist and co-founder of the Medical Freedom and Individual Rights group, said in an email that the gun owners he spoke to “have no understanding of firearm ownership. “I find the questions intrusive in a different way than questions about drug use or sexual partners.” ”
Chesan Sathya, a pediatric trauma surgeon and director of Northwell Health’s Gun Violence Prevention Center, said these topics used to be controversial among doctors. To treat guns as a public health issue, he told me, “it’s not an uncomfortable conversation to have.” However, doctors have more power in this situation than in others. You might tell a diabetic patient to stop drinking soda three times a day, but you literally can’t take soda away from them. If you have a gun, you might be able to do that. In states with extreme risk laws, if a health care provider determines that their patient poses an imminent threat to themselves or others, they may work with law enforcement to temporarily remove someone’s firearm. You can apply to the court to have it removed. A few states allow medical professionals to file these petitions directly. Jake Wiskerchen, a mental health counselor in Nevada, said, “Currently, people across America own guns and are seeking counseling because they don’t want their rights taken away for real or imagined reasons.” There are a lot of people who don’t want to come.” defender For such patients, he told me. They are concerned that if a doctor records gun ownership status in their medical records, they could be added to a hypothetical national registry of firearm owners. And if questions about guns become truly routine in the doctor’s office (such as on medical questionnaires), he said, owners may simply lie or decide they “don’t want to go to the doctor anymore.” Ta.
Therefore, doctors choose their words carefully.they talk about prevention gun injury Instead of gun violenceThat’s because the vast majority of gun deaths are suicides, not murders, and the word doesn’t really mean much. Telling diabetics to reduce their soda intake may help, but people “are not just going to throw their guns in the trash,” said Bernhorst, of the University of California, Davis. “Firearms have far more psychological meaning to people than soda.”
Barsotti said a public health approach to firearm safety requires further engagement with the more than 30 percent of American adults who own firearms. Shooting range and gun store owners are already “practicing public health without the benefit of medical or public health expertise,” he told me.they run themselves storage program For community members who don’t want to carry a gun for whatever reason. They bring their friends in for mental health treatment when they themselves may be at risk. Betts’ team works with gun stores, gun ranges, and law enforcement agencies in Colorado. Firearms storage map She is on the most sites that agree to temporarily hold a gun, and she Colorado Firearm Safety Coalition. Doctor’s office conversations can save lives, but health care workers “have a role to play” in preventing gunshot injuries, Betts said. We are not the solution. ”