As mammals get older, many of us begin to lose sight because the neurons in our retina degenerate. It can be eroded by macular degeneration and retinitis pigmentosa. Somewhere along the course of evolution, we lost the ability to regenerate these types of cells, just as we lost the ability to regenerate limbs. When they are gone, they are gone.

But we humans have developed some other things really well, such as the ability to use reason and the desire to maintain ourselves. It brought us to the brink of making up for it.
That’s amazing enough we can now Grow human stem cells into retinal “organoids”. include All of the different cell types needed to make a functioning retina are organized into appropriate layers.

But now, when we break the organoids down into individual cells, we find that those cells can spontaneously form signaling connections (synapse) with other retinal cells. This means that patients can grow their own stem cells into retinal cells and apply them to their own retina, and these new cells can functionally replace the old cells, restoring vision. no need, thank you very much.
You can read all about this final hurdle overcame in the University of Wisconsin lab of Dr.with David Gumm Zhao Xinyu January 4th issue of Proceedings of the National Academy of Sciences.
Just last year, Gum’s laboratory Indicated Rods and cones (photoreceptors) made from stem cells can respond to light in the same way as healthy cells. This is a great development for making individual cells for therapy, but to become part of a functional retina, these rods and cones need to be able to send signals to the rest of the retina. there is. This is a signaling molecule (mainly glutamic acid) is passed:

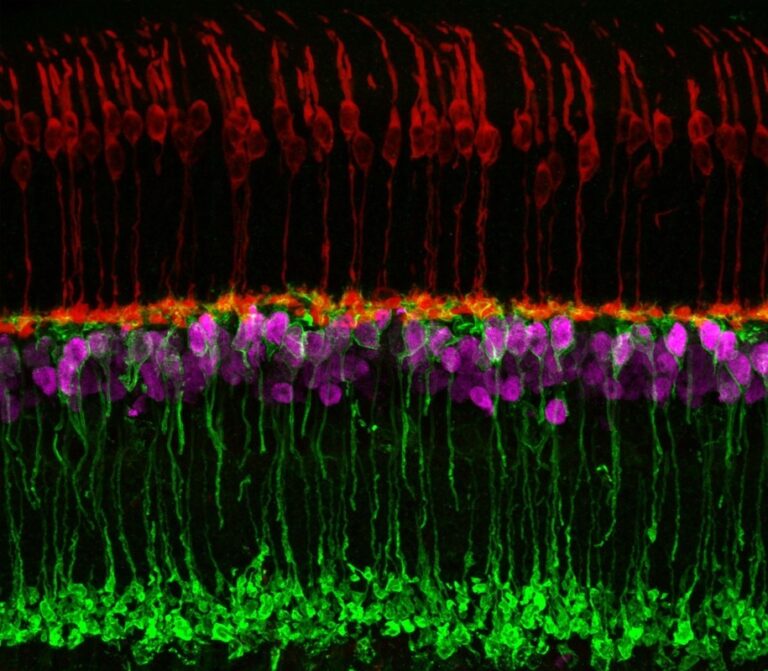
Retinal organoids (ROs) gave Gamm and Zhao hope that stem cells could indeed reconstruct defective parts of the retina. make connections each other within the RO with synapses. We can see how the RO structure resembles the real retina as far as cell types and synapses (stained in green) are concerned.

The question is, if we degrade these RO cells and apply the appropriate RO cells to the patient’s retina, will the patient be able to remake these synaptic connections? That’s what Gamm and Zhao’s lab is trying to test here.
They degraded some RO with papain, the papaya enzyme used as a meat tenderizer and digestive aid, Are known destroy synapses. (Don’t inject papain directly into the eyeball, okay?)

After papain treatment, they confirmed that the proteins important for synaptic function were fortunately still there, but they had returned to the cells. , the cells seemed to have a good shot at re-establishing synapses with each other.
They cultured these RO cells together as individuals on plates for 20 days in a situation similar to that applied to the real retina. But how can we tell that neurons form these tiny synapses and that those synapses are working?
Luckily, there is a clever method called “synaptic tracing.”Rabies virus found to be able to infect between neurons that’s all Through functioning synapses, it can be used not only to find out if synapses exist, but also how well they are functioning. (I think it’s a good time to add the rabies virus to the very long and still growing list of things you shouldn’t inject into your eyeballs.)
Very cool way to do this. You’ll see a colorful photo at the end that makes it very clear what happened, so stick around here.
First, the rabies virus needs to infect a small percentage of the cells without ravaging the entire culture, and you also need to mark those cells as “starters” somehow. there is.
We start with another virus — a lentivirus — that has the gene for green fluorescent protein (GFP) targeted to the nucleus. Lentivirus-infected cells can be found by the large green dot in the center. The amount of lentivirus used can be trial-and-errored to infect approximately 5% of the cells.
Two other genes called TVA and Rgp are inserted into the lentivirus. I’ll quickly explain why both of these are important.
The rabies virus then infects the cell, but alters the gene for its coat protein. It’s usually Rgp, but replace it with something else called Env. Viruses that use Env as their coat protein can only infect cells with TVA. This is exactly why we put TVA in the green dot cells. Now, when the rabies virus is scattered in the culture medium, it will infect only the cells with green dots.
By incorporating the gene for mCherry (red fluorescent protein) into the rabies virus, cells infected with it become red throughout, making rabies-infected cells easy to spot. So all of our green-dotted ‘starter’ cells have TVA, so they all become infected with rabies, turning the ‘starter’ cells celebratory red and green.
Recall that we also incorporated the Rgp gene into the lentivirus. So the green dot cells also make her Rgp protein. When the rabies virus infects our green dot cells, they regain their original coat proteins and revert to their original selves.
So currently about 5% of our cells are red and green ‘starter’ cells that can infect other cells in culture with rabies (and give them their red color). Only if they are connected to other cells by working synapses! In that case, you should see red blood cells without green dots, i.e. rabies-infected cells that are not starter cells. Bam! I have your visualization. So let’s get down to it…
A good control to start with is the whole system just described, but lentivirus has no Rgp. This means that rabies does not have a normal coat protein, so the starter cells should not be able to infect other cells.
The small figure on the bottom left shows that red and green starter cells cannot infect other cells even with active synapses. All cells are displayed in blue, as the DNA of the In this way, the percentage of cells infected as starter cells can be visualized. Then remove the blue DAPI on the right side so only red and green are visible. Note that all red people also have green dots.

So let’s do a real test where Rgp is in the lentivirus to allow the rabies virus to infect other cells, Only through active synapsesThe same goes for colors, and we expect to see red-only neurons.

There is considerable rabies infection of non-starter cells.This means that we have active synapses! to clinical trials!
Gamm, who holds the organoid patent and co-founded Madison-based Opsis Therapeutics, said: It builds on UW-Madison’s findings and adapts the technology to treat eye disorders in humans. “Ultimately, it all leads to the next clear step: human clinical trials.”
After confirming the existence of synaptic connections, the researchers analyzed the associated cells and found that the most common retinal cell types that form synapses were photoreceptors (rods and cones). They are also lost in diseases such as retinitis pigmentosa and age-related macular degeneration. Like certain eye injuries. Retinal ganglion cells, the next most common cell type, degenerate in optic nerve disorders such as glaucoma.
“This was an important revelation for us,” says Gamm. “It really shows the wide-ranging impact these retinal organoids can have.”