overview: By blocking NMDA receptors, ketamine increases noise to gamma frequencies in one layer of the thalamic nucleus and one layer of the somatosensory cortex. Findings suggest that psychosis may be caused by increased background noise that impairs thalamocortical neurons, which may be caused by dysfunction of NMDA receptors that affect the balance between inhibition and excitation in the brain. suggests.
sauce: HSE
An international team of researchers, including Sofya Kulikova, Senior Research Fellow at HSE University-Perm, has found that the NMDA receptor inhibitor ketamine increases background noise in the brain, increases the entropy of incoming sensory signals, found to disrupt transmission between and thalamus. cortex.
This finding may help advance our understanding of the causes of psychosis in schizophrenia.
A paper summarizing the research results European Journal of Neuroscience.
Schizophrenia spectrum disorder affects approximately 1 in 300 people worldwide. The most common symptoms of these disorders are perceptual disturbances such as hallucinations, delusions, and psychoses.
A drug called ketamine can cause mental states that resemble psychosis in healthy people. Imbalances in central nervous system excitation and inhibition can affect perceptual accuracy.
Similar changes in NMDA receptor function are now thought to be one of the causes of sensory disturbances in schizophrenia. is still unknown.
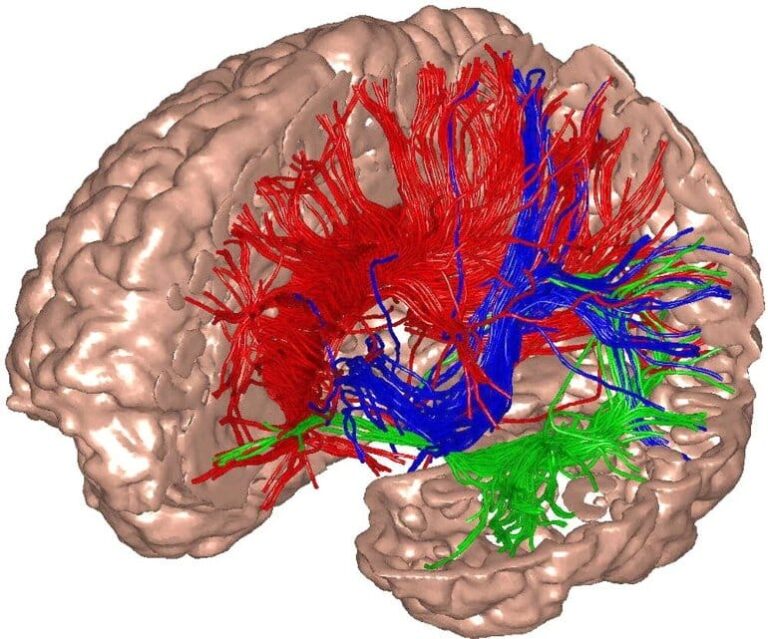
Neuroscientists from France, Austria and Russia have examined how the brains of laboratory rats fed ketamine process sensory signals. Researchers examined beta and gamma oscillations in the thalamocortical system (the neural network that connects the cerebral cortex and thalamus) of the rodent brain in response to sensory stimuli. This neural network is involved in the transmission of sensory information from the sensory organs to the brain.
Beta oscillations are brain waves in the range of 15-30 Hz and gamma waves are brain waves in the range of 30-80 Hz. These frequencies are thought to be important for the encoding and integration of sensory information.
In the experiment, they implanted microelectrodes in rats to record electrical activity in the thalamus and the somatosensory cortex, the region of the brain responsible for processing sensory information from the thalamus. Researchers stimulated rat whiskers and recorded brain responses before and after ketamine administration.
Comparing the two datasets, ketamine increased the power of beta and gamma oscillations in the cortex and thalamus even in the resting state before stimulus presentation, and the amplitude of beta/gamma oscillations decreased 200–700 ms after presentation of the stimulus. revealed to have increased. Duration of stimulation was significantly shorter in all cortical and thalamic sites recorded after ketamine administration.
A post-stimulus elapsed time of 200–700 ms is long enough to encode, integrate, and perceive incoming sensory signals. The observed reduction in vibrational force evoked by sensory stimuli may be related to perceptual disturbances.
Analyzes show that by inhibiting NMDA receptors, ketamine administration can also add noise to gamma frequencies in one thalamic nucleus and one layer of the somatosensory cortex for a period of 200–700 ms after stimulation. It became clear. It is conceivable that this observed increase in noise, or decrease in signal-to-noise ratio, also indicates an impaired ability of neurons to process incoming sensory signals.
These findings suggest that psychosis may be induced by increased background noise that impairs thalamocortical neuron function. This may be caused by dysfunction of NMDA receptors, which affect the balance between inhibition and excitation in the brain. Noise weakens the definition and pronunciation of sensory signals. In addition, this can trigger spontaneous outbursts of activity associated with a distorted perception of reality.
“The discovery of alterations in thalamic and cortical electrical activity associated with ketamine-induced sensory information processing disorders may be useful in testing antipsychotic drugs and predicting disease course in patients with psychotic spectrum disorders. It could be useful as a biomarker for
About this neuroscience research news
author: Anastasia Lobanova
sauce: HSE
contact: Anastasia Lobanova – HSE
image: Image credit to Izikevic, Edelman
Original research: open access.
“The psychomimetic drug ketamine disrupts transmission of late sensory information in the corticothalamic network” by Yi Qin et al. European Journal of Neuroscience
overview
The psychomimetic drug ketamine disrupts transmission of late sensory information in the corticothalamic network
In prodromal and early schizophrenia, deficits in attention and perception are associated with structural and chemical abnormalities in the brain and dysfunction of the corticothalamic network, which is indicative of brain rhythm disturbances. The underlying mechanisms are elusive.
Ketamine, a noncompetitive NMDA receptor antagonist, has been shown to affect prodromal and prodromal phases, including impairment of ongoing and task- and sensory-related broadband beta/gamma frequency (17–29 Hz/30–80 Hz) oscillations in the corticothalamic network. Simulate early schizophrenia symptoms.
In normal healthy subjects and rodents, complex integration processes such as sensory perception undergo transient large-scale synchronization in timeframes of hundreds of milliseconds (200–700 ms) after presentation of an object of attention. Induce beta/gamma oscillations (e.g. sensory stimulation).
Our goal was to use an electrophysiological multisite network approach to investigate the effect of a single dose of the psychomimetic ketamine (2.5 mg/kg, s.c.) on sensory-induced oscillations in lightly anesthetized rats. was to investigate.
Ketamine transiently increased the power of baseline beta/gamma oscillations and decreased sensory-evoked beta/gamma oscillations. Furthermore, it disrupted signal transduction in both the somatosensory thalamus and associated cortices, and decreased sensory-evoked thalamocortical connectivity in the broadband gamma range.
Current findings support the hypothesis that NMDA receptor antagonism disrupts the transmission of sensory information in the somatosensory cortico-thalamo-cortical system.