Researchers who have pieced together the pieces of Alzheimer’s disease’s giant puzzle are closer to slipping the next piece into place, creating yet another connection between our internal organs and our brains.
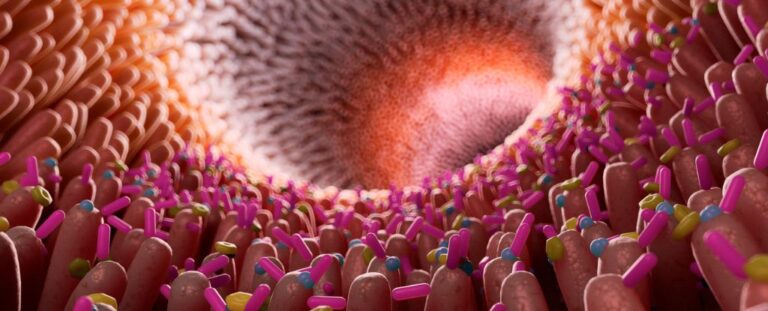
Recent animal studies have demonstrated that Alzheimer’s disease can be transmitted to young mice through gut microbial transmission, confirming the link between the digestive system and brain health.
New research further supports the theory that inflammation may be the mechanism by which this occurs.
“We showed that people with Alzheimer’s disease had more enteritis, and when we did brain imaging studies of Alzheimer’s patients, we found that people with more gut inflammation had higher levels of amyloid plaque accumulation in their brains. It was expensive.” To tell Barbara Bendlin, a psychologist at the University of Wisconsin.
University of Wisconsin pathologist Margo Heston and an international research team fecal calprotectin‘Alzheimer’s disease signatures’ – signs of inflammation – were detected in stool samples from 125 people from two Alzheimer’s disease prevention cohort studies.
Participants underwent several cognitive tests during enrollment, as well as interviews about family history and testing for high-risk Alzheimer’s disease genes. Some subjects underwent laboratory tests for signs of amyloid protein clumps, a common sign of ongoing pathology that causes neurodegenerative conditions.
Calprotectin levels were generally higher in older patients, but were even more pronounced in patients with the characteristic amyloid plaques of Alzheimer’s disease.
Levels of other Alzheimer’s disease biomarkers also increased with levels of inflammation, and memory test scores also decreased with an increase in calprotectin. Even in participants who had not been diagnosed with Alzheimer’s disease, higher calprotectin levels were associated with lower memory scores.
“We cannot infer causation from this study. For that we need to conduct animal experiments.” Note Heston.
Laboratory analyzes have previously shown that chemicals in gut bacteria can stimulate inflammatory signals in the brain. Moreover, Other research They found that intestinal inflammation was increased in Alzheimer’s patients compared to controls.
Heston and colleagues suspect that changes in the microbiome may trigger changes in the gut, leading to systemic inflammation. This inflammation is mild but chronic, causing subtle gradual damage that ultimately interferes with the sensitivity of our body’s barriers.
“Increased intestinal permeability can lead to increased blood levels of inflammatory molecules and toxins originating from the intestinal lumen, leading to systemic inflammation that compromises the blood-brain barrier and It can promote inflammation and potentially promote neuronal damage and neurodegeneration.” To tell Federico Rey, a bacteriologist at the University of Wisconsin.
Researchers are currently experimenting on mice to find out whether dietary changes associated with increased inflammation can cause Alzheimer’s disease in rodents.
Despite decades of research, there is still no effective treatment for the millions of Alzheimer’s patients worldwide. But as our understanding of biological processes improves, scientists are inching closer.
This research scientific report.