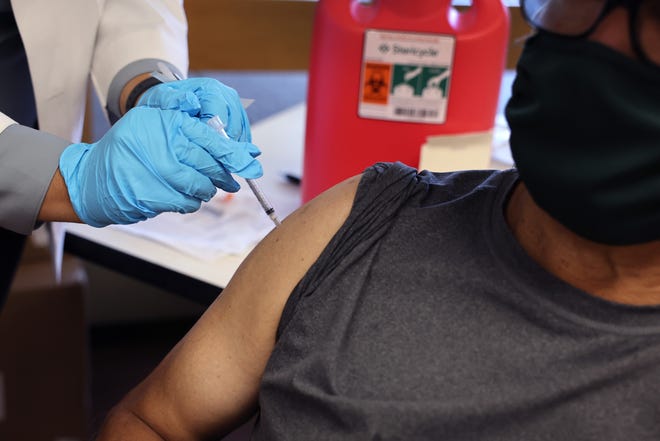
When COVID-19 vaccines entered the commercial market last fall, the federal government created a program to help people with limited coverage or the uninsured get vaccinated. Introduced. The program, which provided millions of free shots to low-income people, is now being shut down, U.S. health officials say.
The Bridge Access program is set to end in August, several months earlier than local health departments and health centers had anticipated, as pandemic-era funding from Congress expires. Biden administration officials are seeking permanent funding to ensure routine vaccinations for adults would continue to be free through a program similar to the long-running “Vaccines for Children” program, a CDC official said in an email.
Access to health:Imagine what would happen if the government provided dental care. A new federal rule could make that a reality.
Health center and department leaders were not above speaking out. bridge access program, they are concerned about how to secure funding for vaccines in preparation for the winter respiratory virus season, when hospitalizations and deaths tend to increase. Many low-income Americans may not be able to afford vaccines against the new coronavirus and its myriad variants. Modern vaccines targeting these strains will be developed, but pandemic-era funding will be lost.
“Money isn’t infinite, but COVID is still with us,” said Whittier Street, a federally qualified health center serving primarily Boston’s low-income communities of color. – said Frederica Williams, CEO of the Health Center. The program leverages Bridge Access funding to administer vaccines.
About a fifth of the center’s patients are uninsured, including many immigrants from Haiti and Latin America, Williams said. That doesn’t include ride-share drivers, restaurant workers and others who have health insurance but don’t have coverage for the vaccine.
Last fall, CDC Director Dr. Mandy Cohen Visit Whittier Street Health Center To facilitate updated COVID-19 vaccines, the health center has launched the Bridge Access Program. Mr. Williams was surprised by the sudden end to his funding. As of this week, the health center had not received any notice of the end of the Bridge Access program, she said.
Leaders of the National Association of Community Health Centers, a nonprofit advocacy group, said they knew the program was temporary but were surprised to hear it would end this August. Sarah Price, the association’s director of public health integration, said in a statement that health centers will continue vaccinating people daily as this cold season brings an increase in looming respiratory illnesses like influenza, RSV and COVID-19. “Health centers will either stock these vaccines or refer them to resources within their communities, with the goal of addressing access barriers and closing the loop,” she said.
Since its launch on Sept. 13, 2023, Bridge Access has provided more than 1.4 million doses of COVID-19 vaccines at no cost through pharmacies, community health centers and public health departments across the U.S., Centers for Disease Control and Prevention (CDC) spokesman David Daigle said in an email. The CDC did not respond to a question about whether it had informed health centers and public health departments that the Bridge Program would end in August.
“Beginning in August, there may be a small amount of free vaccine available through the Health Department’s vaccination program, but supplies are very limited,” Daigle said in the email, which was first shared on social media. CBS news reporter“It remains to be seen whether manufacturers will implement patient assistance programs.”
Vaccine makers Novavax and Pfizer said in an email that they plan to evaluate accessibility options for U.S. consumers in response to the changes and ensure that uninsured and underinsured patients have access to the vaccine. he said in an email. Moderna did not respond to a request for comment.
When a federal panel broadly recommended an improved version of the vaccine in September, many people hit a wall trying to pay for it. Major pharmacies in the US were charging more than $100 per dose. At the time, the Bridge Access Program was a pioneer in providing vaccinations to people who couldn’t afford it, and was cited by many on social media.
With the end of the program, health officials are concerned about an increase in the number of infections.
“This is creating barriers that are going to lead to a bigger resurgence of COVID,” said Dr. Walter Orenstein, associate director of the Emory University Vaccine Center, who previously served as director of the U.S. National Immunization Program. Vaccine programs for children started in the 1990s And he predicts problems will arise if vaccines are not made more accessible.
“I hope I’m wrong, but I think it’s better to remove barriers to access to vaccination than to make people unwilling to get vaccinated when there is a safe and effective vaccine.”
mental health:How to prevent suicide? A place to call home, people to contact
The number of uninsured people in the United States hits an all-time low. Ministry of Health and Human Services Announced in August. But about 7.7% of the population, or about 25 million people, still lack health insurance. Among adults 18 and older, 11% are uninsured. Experts say many of the uninsured are people of color and immigrants. The uninsured also tend to be younger, have lower incomes and live in southern states that have not expanded access to Medicaid. This demographic group also includes millions of undocumented immigrants who do not qualify for federal health insurance.
Additionally, millions of adults have underinsured health insurance through their employers, and many earn too much to qualify for Medicaid. These categories of people would likely have had a harder time receiving a COVID-19 vaccine without Bridge Access funding.

Vaccine funding is ending as Medicaid is cut across the United States. Approximately 22 million people who were enrolled in Medicaid during the pandemic have been disenrolled as of May 10th. KFFa nonpartisan health policy organization.
North Carolina is an exception, with the state legislature expanding Medicaid to adults at the end of 2023. The decline in Medicaid enrollment in the state is smaller than in other parts of the country. The state paid for the preventive vaccines, said Raynard Washington, public health director for Mecklenburg County, which includes Charlotte.
About 13% of the county’s adult population is uninsured, Washington said. These patients are disproportionately Latino and foreign-born. Many of the people vaccinated in the county have jobs that don’t provide benefits or have incomes high enough to preclude them from receiving Medicaid.
Washington, who chairs the Metropolitan Health Coalition, a consortium of top U.S. health officials, believes Congress should work to improve the public health system instead of chipping away at efforts put in place since the pandemic. There is. He said it’s important to invest in vaccines to protect yourself and yourself.
He said it was important to invest in vaccines to protect ourselves and others at risk of severe illness.
“Of course, we know that with COVID-19, some people are still susceptible to severe illness,” Washington said, “so these vaccines, in many ways, are going to save some people’s lives.”
The Washington coalition has supported the Biden administration’s vaccine proposal for adults, but it has not yet been passed.
This is not the time to let up on COVID-19 prevention, he said.
“We have to invest in times of crisis and times of non-crisis,” he said.
The next coronavirus vaccine targeting the dominant strain has not yet been released. If released, Washington expects local and state officials to pay for it with other sources.
Williams said she recently received a call from two patients at Boston’s Whittier Street Center who had tested positive for COVID-19.
Williams met a Haitian man and woman through a program at a local church who asked about antiviral medications they could get through the state’s public health department. They were uninsured. She said the program they were asking about ended in March, but the Whittier center would cover their treatment regardless of insurance.
Even if the pandemic eases, the need for care will still remain, she said.
“We have to find a way to stay true to our mission as we have always been,” she said.