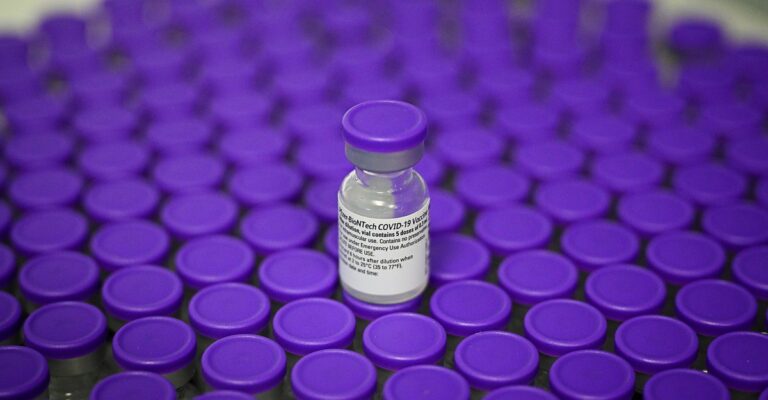
This fall, millions of Americans may line up for yet another type of coronavirus vaccine. It is the first vaccine to lack the strain that caused the pandemic more than three and a half years ago. Unlike the current bivalent vaccine, which protects against two variants at once, the next vaccine may contain only one major component, similar to the first version of the vaccine. It is the spike protein of his XBB.1 lineage, one of the most famous Omicron mutants in the world. Current dominant clade.
The plan has not yet been decided. The FDA still has to convene a panel of experts, after which it plans to make a final decision on the recipe next fall. But some experts have told me they hope government agencies will follow suit. Recent Recommendations of the World Health Organization Advisory Group And the next vaccine will focus only on currently circulating strains.
Switch strategy — from two variations to one variation, Original SARS-CoV-2 and Omicron To XBB.1 aloneExperts told me this would be a serious but wise move. This reflects the world’s latest understanding of viral evolution and immune system idiosyncrasies. “This makes a lot of sense,” said Melanie Ott, director of the Gladstone Institute of Virology in San Francisco. XBB.1 is the major coronavirus group currently circulating. Neither the original variant, nor BA.5, the two coronavirus flavors included in the bivalent shots, are meaningful anymore. And a vaccine focused on XBB.1 could be particularly effective in expanding immunity to people around the world.
At the same time, the COVID-19 vaccine is still in beta testing. Over the past three years, the virus has spawned countless iterations, many of which are very good at outwitting us. Meanwhile, we humans are only his third attempt at designing a vaccine that can keep up with the speed of pathogen evolution. And Emory University immunologist Rafi Ahmed says we’re still learning about the coronavirus’s flexibility and ability to change. It has long been clear that vaccines are essential to prevent serious illness and death, and that some rate of booster vaccination is probably necessary to keep vaccines highly effective. But as viruses change their evolutionary strategies, our vaccine strategies must follow suit. And experts are still racking their brains about how to account for those changes when choosing annual vaccinations.
In the spring and summer of 2022, when the United States was last considering formulating a new vaccine, Omicron was still relatively new and the evolution of the coronavirus seemed very fluid. For more than two years, the pathogen had sporadically spewed out variants of Greek letters without a clear succession plan. Rather than accumulating genetic changes within a single lineage (a more iterative form of evolution, much like influenza strains do), coronaviruses spawned a plethora of distantly related mutants that vie for control. . Delta was not a direct descendant of Alpha. Omicron was not a Delta derivative. No one can say for sure what will happen next or when. “We didn’t understand the trajectory,” said Canta Subbarao, head of the WHO advisory group convened to make recommendations on a COVID-19 vaccine.
So the experts played it safe. Contains Omicron variants Given how much the virus has changed, this shot felt important. But going all-in on Omicron seemed too risky. Subbarao said some experts were concerned that “the virus could flip to an alpha, delta, or something else-like variant.” As a compromise, several countries, including the United States, have adopted a half original, half Omicron combination in an attempt to reactivate OG immunity while developing new defenses against the strains circulating daily. .
and those shots bottom Similar to boosters, it strengthens existing immunity. But it didn’t spark the new wave of responses to Omicron as some experts had hoped, Ott said. The bodies of those already trained on the ancestral version of the virus seem to have become a little short-sighted. It repeatedly awakened its defenses against past viruses at the expense of new viruses that could attack Omicron more forcefully. Subbarao told me that the results were never considered harmful. “For example, the bivalent vaccine still broadened people’s immune response to SARS-CoV-2 compared to, say, the original recipe of the vaccine given at a different dose. Effective in reducing hospitalization rates. But in retrospect, Ahmed said he wondered if the Omicron-only boost could have made an already powerful effect even greater.
Getting serious about XBB.1 now will prevent the world from falling into the same trap twice. Those who received the latest vaccine with only that strain would receive only new and unfamiliar ingredients, allowing their immune systems to focus on fresh ingredients and potentially breaking out of the rut of their ancestral strains. The spike protein of XBB.1 is also not diluted with that of older variants. This is Ahmed’s concern with the current bivalent shot. When researchers added omicron to vaccine recipes, The total amount of spike protein did not double.they made up for half of what was there before. Vaccines therefore had only half of the omicron-focused mRNAs they would have had if they had had a monovalent vaccine, and probably had a blunter antibody response.
Recent works Researchers in the lab of Vineet Menachery, a virologist at the University of Texas Medical School, suggest another reason why half-shots of Omicron didn’t provide enough immunity. Subvariants of this lineage, such as BA.5 and XBB.1, have at least one mutation that destabilizes the spike protein and may persist longer than other versions of the spike protein for full learning. considered to be low. immune cells. Especially with bivalent vaccines, the immune response may be biased toward non-omicron components, exacerbating the tendency of already vaccinated people to focus their energies on ancestral strains. For the same reason, monovalent he XBB.1 may not be able to deliver the expected immunizing dose, Menachery said. But if people accept it (still a big problem) If), hospitalization rates among those receiving the latest vaccines are still low, so annual all-strain switching may be selected for next year’s vaccine as well.
Removing ancestral strains from vaccines is not without risks. It is possible that the virus produces a variant that is completely different from her XBB.1, but that seems unlikely at this time. Omicron endured for a year and a half, making it the longest-lived single Greek letter variant since the pandemic began. Even subvariants within the Omicron family appear to sprout into each other more predictably. Leo Poon, a virologist at the University of Hong Kong, says that after a long period of instability, the virus’s shape-shifting is now “less erratic”. Now that the population is covered by a relatively stable immune layer, this may indicate that humanity and the virus have reached de-escalation. Moreover, even if the descendants of rogue Alphas and Deltas rise up, the world is not completely caught off guard. With so many people hoarding defenses against those and other past variants, they’re probably still well buffered against the worst of Covid-19. Acute consequences. (However, that reassurance doesn’t apply to people who still need the first dose, including children who come into the world every day. An XBB.1 boost may be a great option for people who are already immune. However, bivalent vaccines may be a risk-averse option for those with an immunological blank slate, providing broader coverage.)
Further changes in vaccination strategies will undoubtedly occur. SARS-CoV-2 is still a new disease for us. So are our shots. However, the evolution of recent viruses has become more flu-like, with transmission patterns becoming a little more seasonal. U.S. regulators have already announced that a new coronavirus vaccine will likely be offered each fall, similar to the annual flu shot. Viruses are not exactly the same. But as the years go on, comparisons between the new coronavirus and flu vaccinations may become even more pertinent — coronaviruses, for example, have also begun to generate multiple, genetically distinct strains that circulate at the same time. case. In that case, simultaneous vaccination against multiple versions of the virus may be the most effective defense.
Influenza vaccination can be a useful template in another way. These immunizations have followed much the same guidelines for many years, with experts meeting twice a year to decide whether and how to update vaccine ingredients each fall, but these immunizations also needed some flexibility. . Until 2012, vaccines were trivalent and contained components that immunized him against three different strains at once. Many strains, including all of them in the United States, are now tetravalent, and soon, based on new evidence, researchers may call for them to revert to his three-strain recipe. At the same time, influenza and COVID-19 vaccines have major drawbacks. The ingredients in our injectables are selected months before the injectables actually reach us, leaving our immune system to lag behind the blazing virus in the meantime. . Until the world has something more universal, our vaccine strategy will have to fall behind the curve to keep up with the evolutionary whims of these pathogens.